-
August 24, 2021
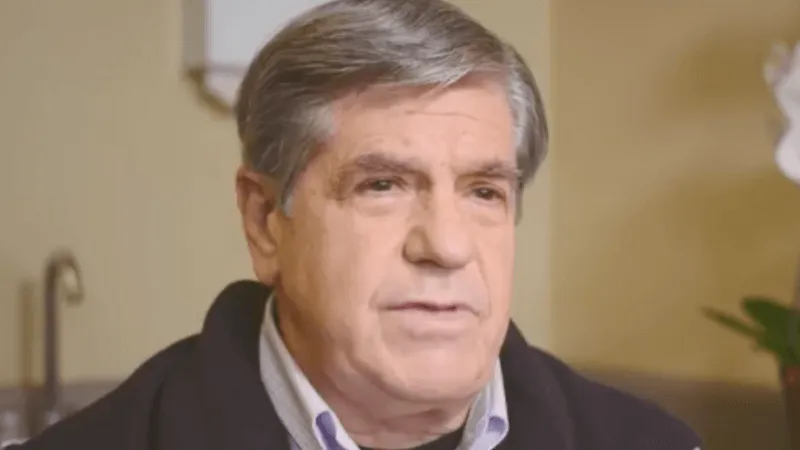
Marc’s Diabetic Feet Beat Part 3: Back to the Present
The third installment of Marc's narrative describing how he manages his diabetes and health challenges.

A Recap
In the first, introductory, installment of my blog, I included a then-current X-ray and picture of an open wound on my left foot. I expressed my intention to describe chronologically in subsequent installments the history and progression of my diabetes that led to the Charcot collapse of my foot and other limb-threatening complications, including the most recent one. In the second installment, I described the circumstances surrounding the onset of the disease. My intention was to describe in this installment the history of my failed effort to control the disease which set the stage for the complications that followed. However, given that most of my readers are already suffering severe foot complications, I have decided to interrupt the chronology of my struggle with diabetes in hopes that a description of the source and treatment of my current problem will be of more immediate value to others who are facing similar challenges.
Diabetic Foot Damage, Neuropathy, and Infection
In my experience, diabetes pitches three strikes against the feet: diabetes compromises the immune system, interferes with circulation, exacerbates dry, cracked skin, and causes fractures and other bone damage that, in turn, results in open sores, fissures, ulcers, and foot collapse. Neuropathy deprives the nerves of sensation that thereby prevents the diabetic from recognizing the presence of injury and taking prompt steps to treat it. An untreated wound is exposed to the risk of serious infection. Infection is the principal threat to the loss of use or, worse, amputation of the diabetic foot.
Prevention...Helps
As I will discuss in detail in later installments, there are a variety of steps that can be taken to prevent the occurrence or limit the severity of foot injuries. They include, in addition to good glucose control, avoiding stressful foot activity and fracture risk, daily foot inspections, wearing well-fitting shoes and/or specialty footwear and orthotics, using anti-callous creams, wearing Siren Socks for early ulcer detection, regular podiatric visits, and prompt treatment of callouses and open wounds. After years of neglect, I have become ardent about following these measures. But, as I am about to describe, they are no guarantee against serious problems. In fact, in this case, one of my efforts to prevent a problem inadvertently precipitated one!
Just a Little Callus
Because calluses can break down and turn into ulcers, preventing and treating them should be a part of the diabetic’s daily foot monitoring and regular visits to the podiatrist. I try to examine my feet at a set time each day and schedule routine podiatrist visits every four to six weeks. While diabetics can help avoid or eliminate calluses by applying specialized creams and ointments, the more troublesome ones require podiatric attention. Podiatrists treat calluses by safely sanding or filing down the callused skin or, in some cases, by debriding them—trimming or excising the callus with a blade or scalpel. Both methods are normally safe, relatively painless, and generally successful. However, even this simple procedure can prove problematic for people suffering from diabetic foot disease. My case in point.
During a routine visit late last year, my podiatrist debrided what he described as a “little callus” on the bottom of my midfoot (interestingly in an area where I do not normally experience ulcers). The incision was small and unremarkable. He told me to keep it covered with a fresh Band-Aid. Because this was the only problem he discovered during the visit, he told me that, unless I noticed signs of infection or other issues, I did not need to return for six weeks. (Signs of infection include a foul smell, pus, swelling, pain, and warmth around the wound).
Consistent with the podiatrist’s advice, I changed the Band-Aid daily, tried to avoid walking without shoes or otherwise exposing my foot to sources of infection, inspected the callused area periodically, and monitored it for signs of infection. Regrettably, these steps proved inadequate. Four weeks later, I woke up one morning with pain and swelling in my midfoot and observed that the area around the wound was red, contained pus, and was warm to the touch. More alarming yet, I had a 101+ degree fever—an ominous sign of a potentially serious systemic infection. I was rushed to the emergency room of a nearby medical center, diagnosed with a Staph infection, spent five days in the hospital and, despite state-of-the-art wound care (that I will describe in the next installment), am not fully healed and remain mostly non-weight-bearing six months later.
Although at the time the use of a Band-Aid and the precautions that I took seemed to be a reasonable treatment for “a little callous”, in retrospect, they did not protect me from what otherwise might have been potentially avoidable complications.
Next time: Finding state-of-the art wound prevention and treatment.
About Siren Socks
Siren Socks are innovative smart socks that detect potential issues with your feet. Siren Socks are an FDA-registered Class I medical device and are for people with neuropathy.
The socks measure your foot temperature. Temperature monitoring has been shown to help prevent diabetic foot ulcers in multiple clinical studies clinical studies over the past 20 years and is considered the gold standard in diabetic foot care.
The information from the socks is monitored by licensed nurses who contact you regularly to check on your health and the status of your feet. Your doctor review any issues that arise and determine if a clinic visit is necessary.
Siren Socks are covered by Medicare, Medicare Advantage, and many private insurance plans.
Interested patients can find a Siren-Certified Provider near them and begin the enrollment process by clicking here.
[comment]
Related Blog Posts
Latest Articles

Siren Raises $9.5M, Led by an $8M Investment from Mölnlycke Health Care to Drive Diabetic Foot Ulcer Prevention and Management
Siren announces investment by Mölnlycke of $8 million to further development and adoption of Siren’s innovative diabetic foot ulcer prevention solution.
About Siren Socks
Siren Socks are smart socks that help detect potential issues with your feet. Siren Socks are an FDA-registered Class I medical device and are designed for people living with diabetes and neuropathy. The socks measure your foot temperature. Temperature monitoring has been shown to help reduce the number of diabetic foot ulcers in multiple clinical studies over the past 20 years and is considered the gold standard in diabetic foot care. The information from the socks is monitored by licensed nurses who contact you regularly to check on your health and the status of your feet. Your doctor reviews any issues that arise and determine if a clinic visit is necessary. Siren Socks are covered by Medicare, Medicare Advantage, and many private insurance plans. Interested patients can find a Certified Siren Provider near them and begin the enrollment process by clickinghere.
